Healthcare advertising just got way more complicated. The CMS 2026 Proposed Rule fundamentally changed what counts as "marketing" requiring approval, and multiple states rolled out AI restrictions that could tank your mental health campaigns if you're not careful.
Here's the thing: 25% of Medicare beneficiaries live with mental illness, and roughly half are enrolled in MA plans. That's a massive audience, but the compliance landscape shifted dramatically this year. One wrong move with your ad copy or AI chatbot messaging, and you're looking at regulatory violations that could shut down entire campaigns.
The New CMS Marketing Reality
CMS completely rewrote the marketing playbook for 2026. They expanded the definition of "marketing" to include any communication that draws attention to a plan, influences decision-making, or affects enrollment decisions: regardless of whether it mentions specific benefits, premiums, or cost-sharing.
Translation? Even your awareness-level ads now need CMS review and approval.
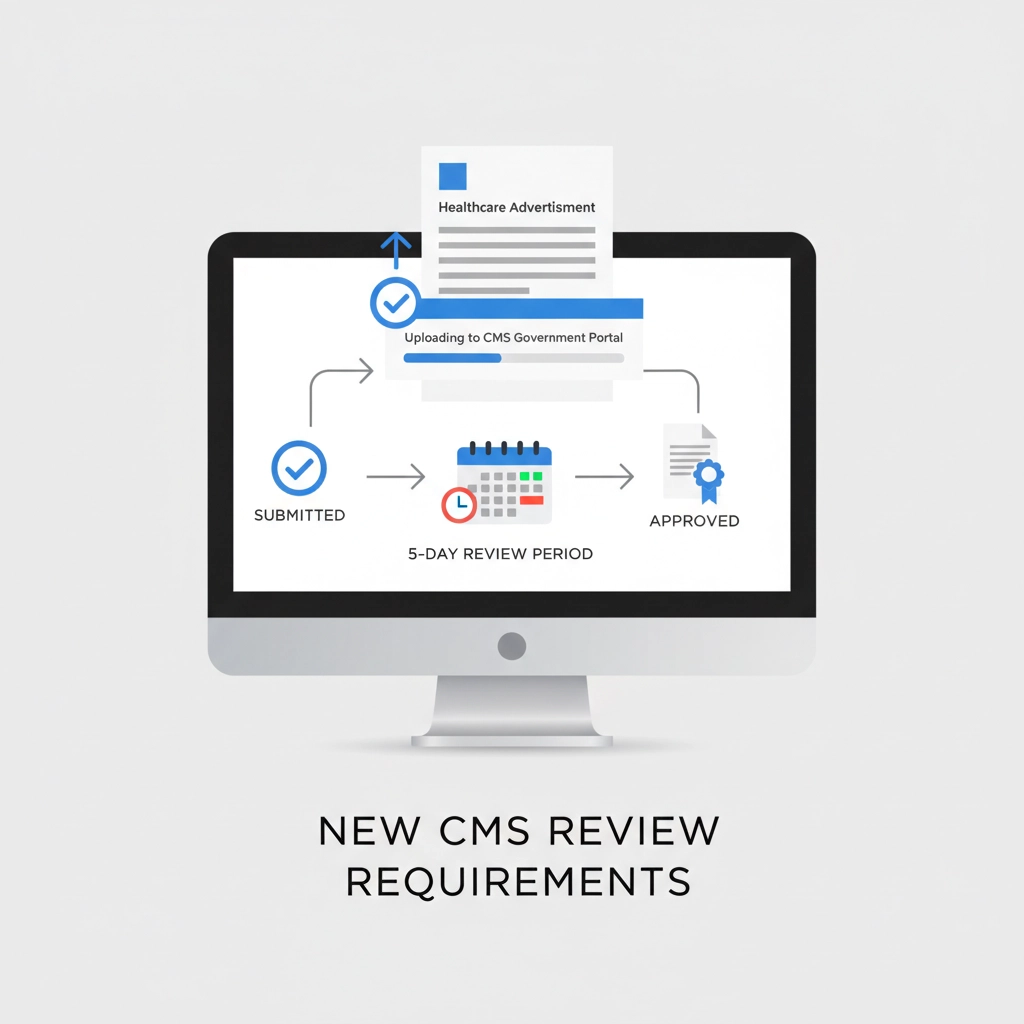
The "File and Use" process lets you submit materials that become usable five days after submission, but CMS made it clear they're providing "stronger oversight" and will move fast on complaints. They're not messing around with non-compliant ads anymore.
What this means for your campaigns:
- Submit ALL marketing materials for CMS review
- Don't rely on old technical loopholes
- Build 5-day approval windows into campaign timelines
- Expect faster enforcement on violations
Supplemental Benefit Marketing Gets Restricted
CMS identified massive confusion around how MA plans market supplemental benefits, especially those debit cards and "flex cards" everyone's been pushing. The new rules prohibit marketing:
- How a supplemental benefit gets delivered (like debit cards)
- The dollar value of supplemental benefits
Those ads suggesting cards "can be used to purchase anything anywhere" or are "automatically received upon enrollment"? They're violations now.
Instead of focusing on delivery methods or dollar amounts, your ads need to highlight the actual benefit itself. Talk about what the benefit does for the patient, not how much it's worth or how it's administered.
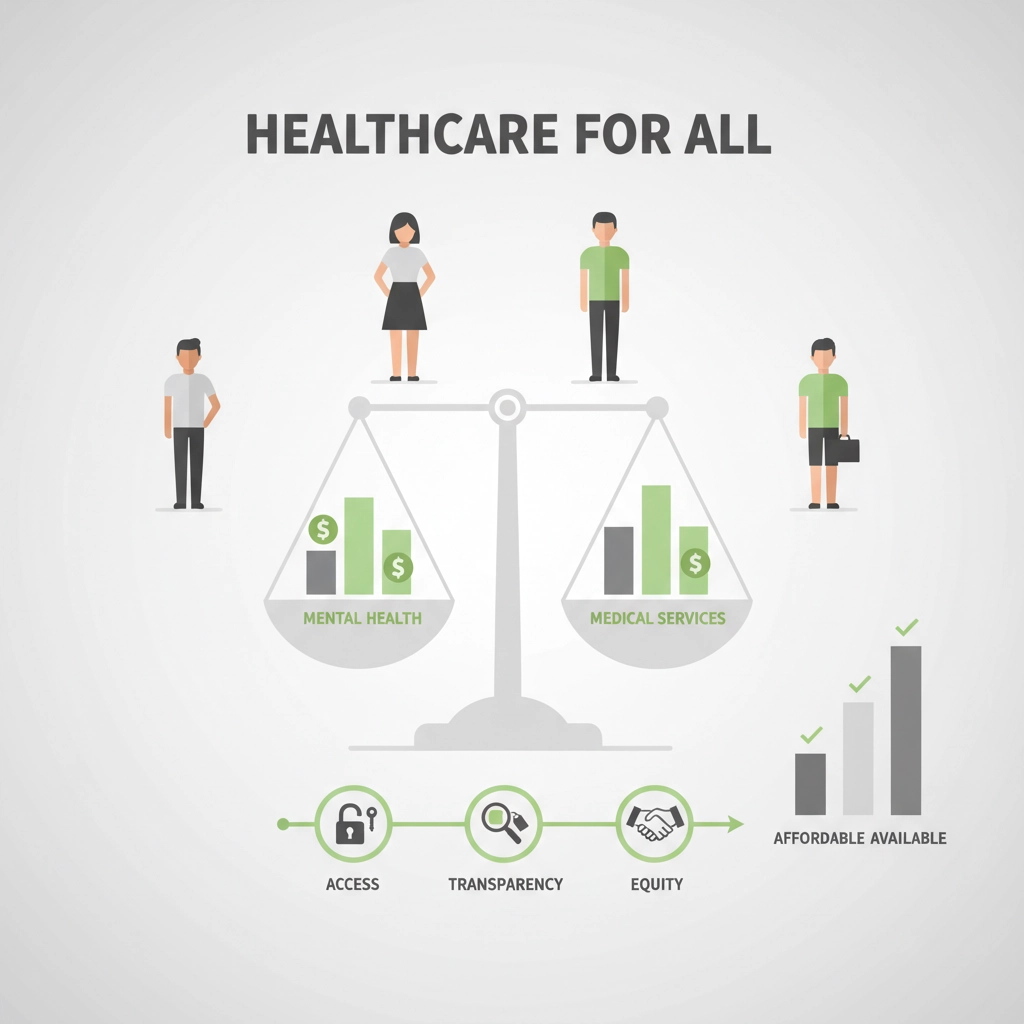
Mental Health Parity Compliance Just Got Strict
The Mental Health Parity and Addiction Equity Act (MHPAEA) requires mental health and substance use disorder benefits match medical/surgical benefits across all six classifications:
- Inpatient/in-network
- Inpatient/out-of-network
- Outpatient/in-network
- Outpatient/out-of-network
- Prescription drugs
- Emergency care
If your plan covers autism treatment like ABA therapy on an outpatient/in-network basis, it must provide that same benefit in all other classifications. No exceptions.
Compliance checkpoint: Before marketing any mental health service, verify your organization offers equivalent coverage across all six benefit classifications. Don't advertise services that aren't available in every required category.
AI Mental Health Restrictions Hit Hard in 2026
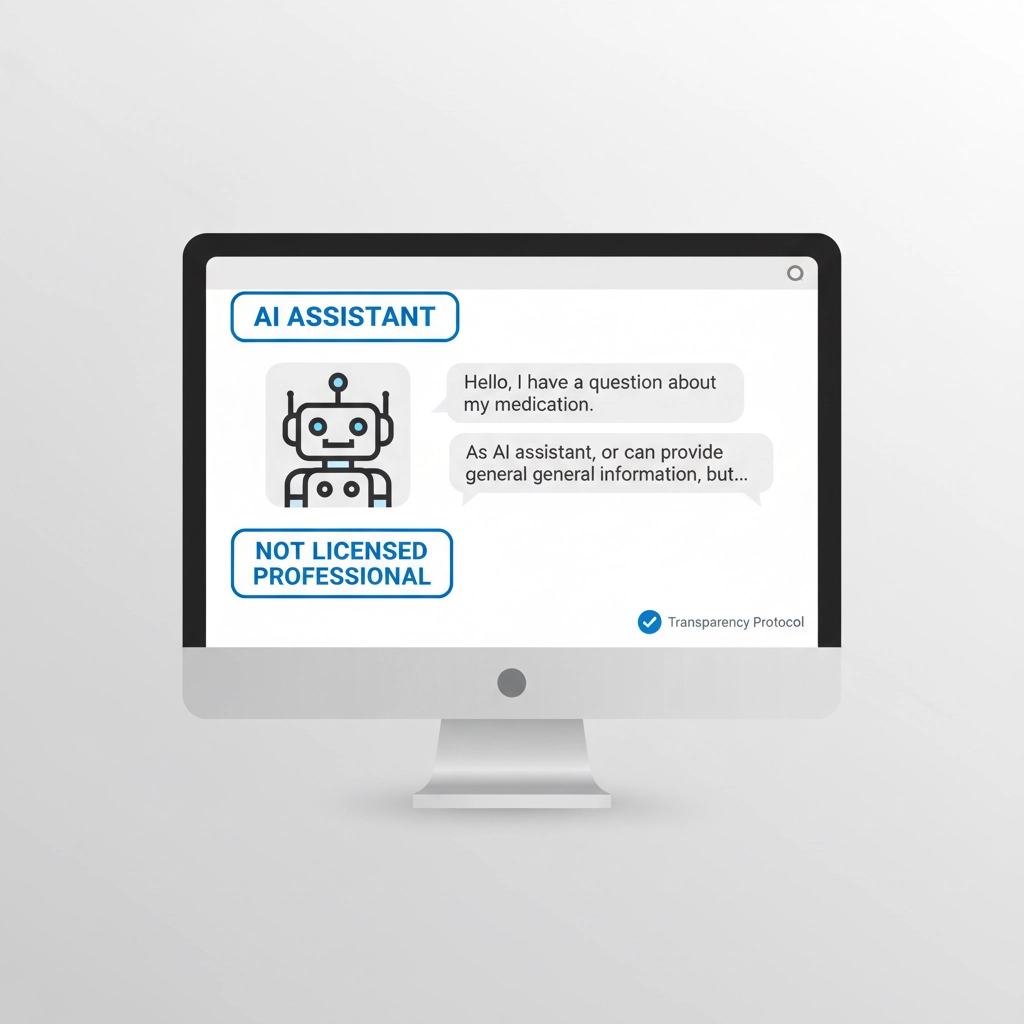
Multiple states dropped the hammer on AI use in mental health advertising. These aren't suggestions: they're laws with real penalties.
Illinois (effective August 1, 2025):
- AI systems can't make independent therapeutic decisions
- No direct AI-client therapeutic communication
- Treatment recommendations require licensed professional review
- Chatbots cannot represent themselves as licensed professionals
California (effective January 1, 2026):
- AI tools cannot indicate they possess healthcare licenses
- No implying care comes from licensed professionals when it's AI-delivered
- Clear disclosure requirements for AI-assisted services
Nevada and Oregon have similar restrictions preventing AI from claiming licensed provider status.
Your AI compliance checklist:
- Never suggest AI services come from licensed professionals
- Clearly disclose AI-assisted or AI-delivered services
- Avoid language suggesting AI has professional credentials
- Ensure licensed professional oversight where required
- Train chatbots to identify as AI, not licensed providers
The Behavioral Health Access Problem
Here's a sobering stat: 23-25% of MA plans impose higher cost-sharing rates for mental health specialty services than traditional Medicare. CMS is pushing hard for equitable access, especially for underserved racial and ethnic groups and low-income communities.
Your behavioral health ads need to clearly communicate cost-sharing rates and prove they're not higher than comparable medical services. This isn't just good practice: it's becoming a compliance requirement.
Advanced Compliance Strategies for 2026
Transparency Requirements
All advertising must include sufficient detail for informed decision-making. CMS specifically called out "simplified advertisements lacking detail needed for enrollment decisions" as violations. Your ads need substance, not just flashy promises.
Beneficiary Complaint Prevention
CMS continues receiving marketing misrepresentation complaints about TV, mail, and internet ads. Review your creative for potential misinterpretations around:
- What services are actually covered
- How and where services can be accessed
- Cost-sharing and coverage limitations
- Pre-authorization requirements
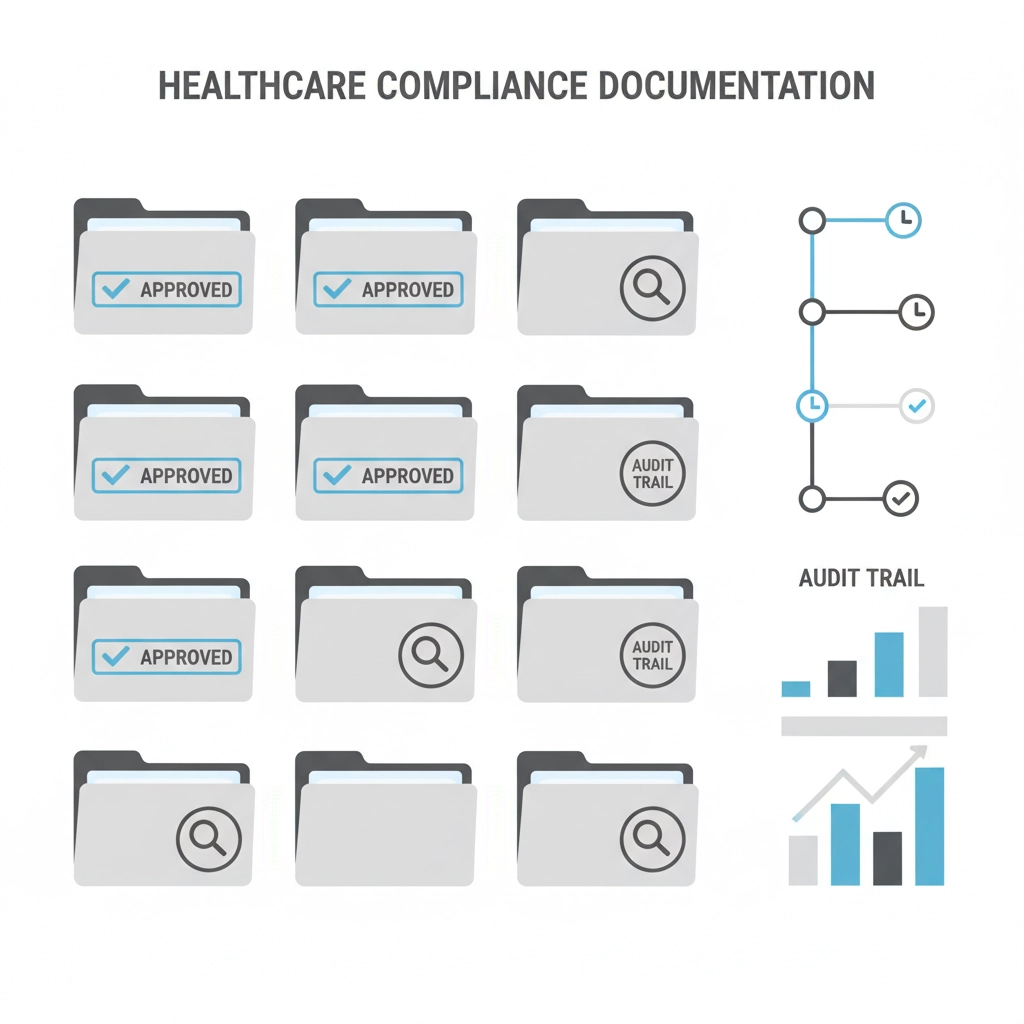
Documentation Standards
Maintain detailed records of:
- All CMS submissions and approval dates
- Compliance certifications
- Post-launch ad modifications
- Beneficiary complaint responses
The regulatory environment is only getting stricter. Having bulletproof documentation protects your campaigns and proves compliance during audits.
Building Future-Proof Healthcare Campaigns
Cross-Functional Review Process
Implement compliance reviews involving legal, compliance, and clinical teams before any ad launches. Claims about mental health parity and behavioral health coverage must be substantiated by your organization's actual benefit structure.
Timeline Management
Build CMS approval windows into every campaign timeline. The days of quick-turnaround healthcare ads are over: factor in submission, review, and potential revision cycles from the start.
State-by-State Compliance Mapping
Create compliance matrices showing AI restrictions and mental health advertising rules by state. What's compliant in Texas might violate California law, and ignorance isn't a defense anymore.
Technology Integration for Compliance
Smart healthcare marketers are building compliance directly into their AI content auditing processes. Automated checks for restricted language, disclosure requirements, and state-specific violations catch problems before they reach regulatory agencies.
The key is having systems that flag potential violations during the creative process, not after campaigns launch. Prevention beats remediation every time in regulated industries.
Moving Forward in 2026
The CMS comment period for the 2026 Proposed Rule closed January 27, 2025, with final rules expected early this year. Monitor CMS guidance updates closely: interpretations of marketing definitions will continue evolving.
Healthcare advertising in 2026 requires a fundamentally different approach. The days of pushing creative boundaries and hoping for the best are over. Successful campaigns now start with compliance and build creative within those boundaries.
The complexity isn't going away. If anything, expect more restrictions as regulators catch up to digital marketing tactics and AI integration. The agencies that invest in compliance infrastructure now will dominate while others scramble to catch up.
Ready to build compliant healthcare campaigns that actually convert? Book a consultation to discuss your specific compliance challenges and campaign goals. The regulatory landscape is complex, but the opportunities for compliant, effective healthcare marketing have never been bigger.